
Article
|
5 mins
|
February 6, 2026
Electronic medical record (EMR) systems, defined as "an electronic record of health-related information on an individual that can be created, gathered, managed, and consulted by authorized clinicians and staff within one health care organization," have the potential to provide substantial benefits to physicians, clinic practices, and health care organizations.
An Healthcare Provider (HCP) is confronted with multiple challenges in the current EMR system:
Interoperability issues: Creates data silos, incomplete longitudinal patient history with non-compliant vendors and tools.
Data security and privacy concerns: Erosion of trust
Clinical resistance for adoption: Workflow disruption with perception of low ROI
EMR systems were designed primarily for discrete, episodic clinical data. There is a new demand to these systems: Ingesting, normalizing, and governing continuous digital biomarkers (Dbx) streams from wearables, home monitoring devices, and other multiomnics sources.
Digital biomarkers (Dbx) are objective, quantifiable physiological and behavioral data collected via digital devices, used to explain, influence, or predict health outcomes.
Dbx data arrives in diverse, high-volume time-series formats that lack uniform coding, complicating mapping to EMR standards like FHIR Observation or LOINC.
Healthcare providers are under pressure to shift from episodic, hospital-centric care to continuous, preventive, and “hospital-at-home” models. EMR systems are central to this shift but were not built to natively handle:
High-frequency time-series data from consumer-grade and near-clinical devices
Heterogeneous payloads and proprietary schemas
Regulatory and standards requirements across jurisdictions (ABDM, US Core, SNOMED CT, LOINC, ICD-10).
Key challenges facing HCP and EMR vendors include:
Interoperability and data silos
Fragmented EMR implementations, non-compliant vendor interfaces, and device-specific portals producing incomplete longitudinal patient records and limiting cross-facility data sharing.
Data security, privacy, and trust
Digital devices often carry electronic Protected Health Information (ePHI) - identifiers, device IDs, IP addresses - raising new consent, access control, and audit requirements.
Clinical adoption and workflow disruption
Clinicians perceive EMR and device integration as high-friction with unclear ROI, especially in high-volume environments typical in India’s Tier-2 and Tier-3 cities.
Dbx explosion and schema rigidity
Traditional EMR schemas optimized for discrete observations struggle with continuous or high-frequency signals, leading to data loss, poor normalization, and weak analytics.
The result is an architecture gap: EMRs must be extended, not replaced, by a scalable, standards-aligned Dbx layer that can integrate with existing systems and comply with local regulations and supporting future international data exchange.
FHIR (Fast Healthcare Interoperability Resource) supports consented data exchange across systems using JSON/XML/RDF, RESTful APIs, while SMART (Substitubtable Medical Applications and Reusable Technologies) provides the authorize and authentication features with OAuth 2.0.
Popular Dbx sources are:
Wearables and patches: Heart rate and derived metrics (HRV, recovery scores) from devices like WHOOP, Garmin, Corsano.
Continuous Glucose Monitoring (CGM): Minute-level glucose from Libre and similar devices.
Voice and audio analytics: Vocal biomarkers for neurological or psychiatric conditions.
Computer vision: Facial analysis for nutritional status, pain, emotion; gait and movement assessment (e.g., VALD-type systems).
ECG, EEG bio signals: Vary from single channel (basic) to multi-channel (12 for ECG for near-clinical Holter like data).
These data streams differ in Sampling frequency, Payload formats, Semantics and Clinical validation maturity. Many will remain adjunctive to clinical decision-making, yet they must be ingested, governed, and made queryable alongside EMR data.
Design principles for any Dbx-EMR extension layer needs to focus on
Standards-first interoperability
Use FHIR R4 as the canonical exchange standard, with regional profiles such as ABDM (India) and US Core as constraints. Map Dbx into FHIR resources like patient, observation, device, deviceMetric, encounter, provenance, bundle
Device-data provenance
Maintain explicit linkage between each data point and its originating device, firmware, configuration, and acquisition context. This enables auditability, traceability, more reliable analytics supporting change of devices or vendors (eliminates vendor locking).
Isolation of concerns
Keep time-series Dbx ingestion and normalization in a scalable data platform and expose a FHIR-compliant interface to EMR systems rather than pushing all raw data directly into the EMR.
Cloud-native scalability
Leverage SaaS services to handle high volume, variable latency, multi-tenant workloads
Regulatory alignment and security by design
Incorporate data protection, consent, and access controls aligned with HIPAA, ABDM guidelines, emerging Indian data protection norms.
A conceptual architecture of a Dbx-EMR extension layer on AWS is discussed below.
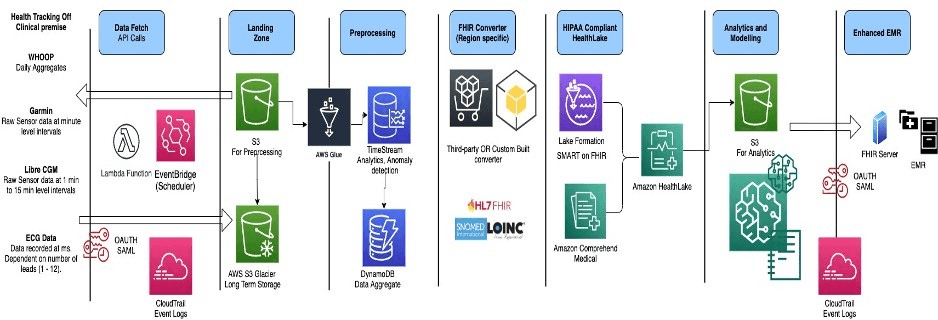
Conceptual AWS Architecture - Focussed on HIPAA/ABDM compliance
Data Fetch Layer - Securely acquire multi-device, multi-frequency Dbx from external APIs. You could use SaaS such as TryTerra or SpikeAPI which contain out-of-the-box APIs for popular devices such as CGM, Smart watches/rings over custom builds (I am biased towards custom builds from a cost consideration and data privacy).
Amazon EventBridge to schedule periodic data pulls (for example, daily for WHOOP summaries, more frequent for CGM or ECG feeds).
AWS Lambda functions to implement adapter logic for each device vendor API.
Integrate vendor OAuth 2.0 flows and SAML/OpenID.
AWS CloudTrail for audit trails.
Device–data mapping: Maintain a device registry (e.g., in Amazon DynamoDB) that links: Patient identifiers (ABHA, MRN, or local IDs), device identifiers (serial, MAC/IMEI if applicable, vendor device ID), Metadata: manufacturer, model, firmware version, acquisition dates
This registry becomes the anchor for device provenance and lifecycle events (activation, deactivation, replacement). It is recommended to be biased towards batched pulls (e.g., once every 6 hours) over high-frequency polling for consumer devices where clinical use does not require real-time alerts.
Landing Zone - Store raw, immutable Dbx as the source of truth.
Raw storage: Use Amazon S3 as a data lake landing zone. Store data partitioned by patient, device, date/time, vendor. NEVER overwrite—use versioning for late-arriving corrections.
Short- and long-term retention: Configure S3 lifecycle policies for hot, warm, cold tiers depending on clinical and analytical needs.
For devices that only allow one-time retrieval of historical data ensure ingestion jobs are Idempotent, robust to retries, never delete the original payload.
This layer ensures that even as downstream schemas evolve, the original telemetry is available for reprocessing, audits, algorithm revalidation.
Preprocessing and Normalization - Clean, standardize, and transform raw Dbx into structured time-series suitable for analytics and FHIR mapping.
Metadata and catalog:
Use AWS Glue Data Catalog to define schemas for each vendor’s payload and harmonized structures. Capture key attributes: Timestamps, units, sampling frequency, channels (for multi-lead ECG), quality flags if available.
Outlier detection and quality checks:
AWS Glue jobs or AWS Lambda-based ETL can: Filter impossible values (e.g., HR > 260 bpm in resting contexts); Flag long gaps or improbable patterns (non-wear, sensor dropout); Normalize units and time zones
Time-series storage:
Store cleaned, structured time-series in Amazon Timestream for performant querying by patient, device, metric (HR, HRV, glucose, etc.)
Use DynamoDB to hold pre-aggregated summaries (Daily statistics, rolling windows, trend flags such as Rolling SDNN over 5-minute windows for the past 7 days; Alerts when glucose remains above a configurable threshold for more than N minutes for rapid access in dashboards or EMR widgets.
FHIR Conversion Layer - Convert curated Dbx into FHIR-compliant resources and Bundles aligned with regional profiles.
Map Dbx elements into FHIR R4 resources
Observation: Dbx values, units, codes (SNOMED CT, LOINC).
Device / DeviceMetric: device metadata and measurement characteristics.
Encounter: link observations to clinical encounters where relevant (e.g., remote follow-up sessions).
Provenance: link data to source device, API call, and timing.
Profiles and localisation:
Implement support for: ABDM FHIR profiles for India (e.g., NDHM-compliant Patient, Encounter, Observation, Document Bundles) for consented exchange via ABDM gateways.
Use either: Third-party FHIR converter solutions from AWS Marketplace (e.g., HiPaaS) configured with ABDM profiles and US Core profiles
OR a custom FHIR conversion microservice that applies StructureDefinitions and Value sets (SNOMED CT, LOINC, RxNorm, ICD-10)
Validation:
Integrate FHIR validators (e.g., HAPI validators, ABDM/NRCeS validators) into CI/CD pipelines and Runtime checks. Reject or quarantine non-conformant resources for review.
The output of this layer is Dbx represented as standards-compliant FHIR resources and Bundles, ready for storage and exchange.
FHIR Storage and EMR Integration - Store FHIR resources securely and expose them for EMR consumption and SMART on FHIR applications.
FHIR data store
Use Amazon HealthLake as a managed, HIPAA-eligible FHIR datastore.
HealthLake Indexes FHIR resources, supports clinical queries Integrates with analytics tools
Security and access control:
Use AWS Lake Formation AWS Identity and Access Management (IAM) and Resource-based policies to implement Role-based access control and Attribute-based access control
Align consent and access with:
o ABDM consent artifacts and policies for Indian contexts.
o HIPAA and local institutional policies elsewhere such as ABDM in India
· SMART on FHIR and EMR interoperability
o Pull Dbx observations or summary documents into patient views
o Launch SMART on FHIR apps that provide Dbx visualizations, and risk stratification
· For EMRs without native FHIR support, build adapter services that:
o Transform FHIR resources into the EMR’s internal schema.
Device–Data Provenance Model
Device provenance is critical when patients switch devices (e.g., from WHOOP 4.0 to a Polar band) or when firmware updates change measurement algorithms.
Experience firmware updates that change measurement algorithms
A robust model should:
Represent devices explicitly as FHIR Device resources, with:
o Manufacturer, model, serial number;
o Firmware/software versions and update timestamps;
o Represent measurement properties in DeviceMetric or Observation extensions (e.g., sampling frequency, filter settings).
Capture acquisition context in FHIR Provenance, linking:
o Observations to originating Device and data-ingestion process.
o Time of measurement vs time of ingestion.
This allows downstream analytics to:
· Differentiate metrics across device generations.
· Recalibrate longitudinal analyses when devices or firmware change.
· Support audits and clinical interpretation in medico-legal contexts. Governance, privacy, and safety considerations
Implement explicit consent workflows for importing Dbx into the clinical record.
Maintain audit logs for access to Dbx, including:
Identity of accessing users
Purpose of access
Exploratory or wellness-grade metrics
Dbx will drive a decisive shift towards preventive care, hospital-at-home models, and advanced analytics at population scale.
EMR systems must rapidly evolve to ingest, normalize, and govern Dbx without compromising interoperability, security, or clinical usability.
Get in touch:
ORANGEHUE LIFE SCIENCES PVT LTD
63/2, Kodichikkanahalli Main Rd, Bommanahalli,
Bengaluru, 560 068 , India
© 2026 OHUE / All Rights Reserved